Safer use of medicines
Medicines are a high volume, high cost, safety-critical intervention, used across all aspects of health and social care. As care continues to become more integrated, sharing of medicines information between sectors, settings and systems is increasingly important.
Supporting safer use of medicines through technology is a strategic priority for NHSGGC and we aim to become a centre of excellence in digital medicines practice.
NHSGGC has made good progress in digitalising medicines practice in recent years: for example, the current rollout of HEPMA will significantly increase NHSGGC digital maturity rating. We now need to build on this to move from islands of good practice to a joined-up patient medication record and integrated medicines practice across NHSGGC and beyond.
Scottish Government and other national organisations are also working to digitalise medicines processes, and NHSGGC is engaging fully with this work to influence the direction of travel. ‘Moving Pharmacy Forward’ is a strategic framework for the development of pharmacy services in NHSGGC. One of the five stated aims is to develop and optimise the use of data and digital solutions.
Our vision is to create a “single source of truth” for patients’ medication. This will bring together medicines information from several sources and present it to clinical staff in a clear and accessible way. Paper-based processes will be digitalised wherever appropriate, with priority given to high volume areas where safety and efficiency benefits can be maximised.
This vision will be achieved by building on and spreading existing capabilities, putting in place strong technical and organisational foundations for future developments, and maximising opportunities to digitalise medicines processes.

Aims:
- Digitalise wherever appropriate
- Reduce clinical risk
- Use medicines more efficiently
- Empower clinical staff to continuously improve practice
NHSGGC will deliver this vision in a series of steps, each of which will deliver tangible benefits to clinical staff and patients, while incrementally building the capabilities required to transform medicines practice across all sectors.
|
Key step |
Example |
|
Spread existing capabilities |
Extend HEPMA to outpatient, day case and other areas |
|
Real-time links for medicines information |
HEPMA/Clinical Portal link for Immediate Discharge Letter |
|
Consolidated view of patient medication |
GP, HEPMA, Clinical Portal, community |
|
Unlock the potential of medicines informatics |
Visual dashboards to inform clinical practice |
The initial phase of HEPMA rollout is focused on inpatient wards and theatres. Future phases will spread the system to outpatient clinics and day case units, and additional opportunities will be considered e.g. oral health. This will extend the breadth of the hospital electronic medicines record and maximise safety and efficiency benefits.
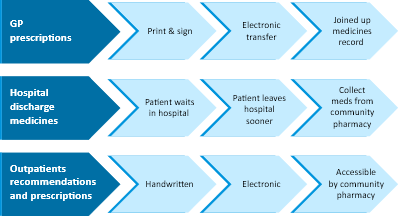
Real-time links between systems will enable electronic sharing of medicines information, reducing the effort and risk associated with manual transcription. HEPMA will link with Clinical Portal to populate the discharge letter medicines list. In later stages we will seek to link GP medicines information with HEPMA.
Medicines and allergy information from multiple sources will be consolidated to give clinical staff a more joined up view of the patient.
Electronic medicines data provides a depth and breadth of detail about clinical practice that was not feasible with paper-based processes. Medicines Informatics will release the information locked up in individual systems and put it in the hands of clinical staff. This will inform and support the day-to-day care of patients and enable ongoing improvements to practice and optimisation of medicines.
Paper-based processes will be replaced with digital alternatives. For example, hospital to GP prescribing recommendations. A new Pharmacy Management System will be implemented fully integrated with HEPMA to enable electronic ordering of medicines by wards.
NHSGGC eMedicines Programme is progressing priority work streams including GP, community and hospital-based services. Key phases are illustrated above. The programme will engage with patients to better understand the citizen perspective on medicines processes, and ensure that the patient’s voice is heard as NHSGGC moves forward.
The Cancer Medicines Outcomes Programme (CMOP) is a national collaboration between the NHS and academia, hosted by NHSGGC, which aims to better understand the outcomes of patients who receive cancer medicines in routine practice in Scotland. ‘Real world data’ (such as information about hospital admissions, test results, prescribed medicines, side effects and demographics) is stored within several record /digital systems. Our aim is to link these data to better understand outcomes in the Scottish population.
